Medically reviewed by Dr. Kanwaljit Singh, MD, Pulmonary medicine Fellowship in Clinical Cardiology, Diploma in Diabetes ECFMG (USA) — Written by Amandeep Singh Vaseer — Updated on December 9, 2025
If you’ve ever experienced a pounding headache and wondered whether your blood pressure might be to blame, you’re not alone. The relationship between high blood pressure and headaches is one of the most common questions patients ask their doctors—and one of the most misunderstood aspects of hypertension.
Here’s what might surprise you: contrary to popular belief, the vast majority of people have no symptoms whatsoever from high blood pressure, including headaches. High blood pressure is often called the “silent killer” precisely because it typically produces no warning signs until it reaches dangerously high levels.
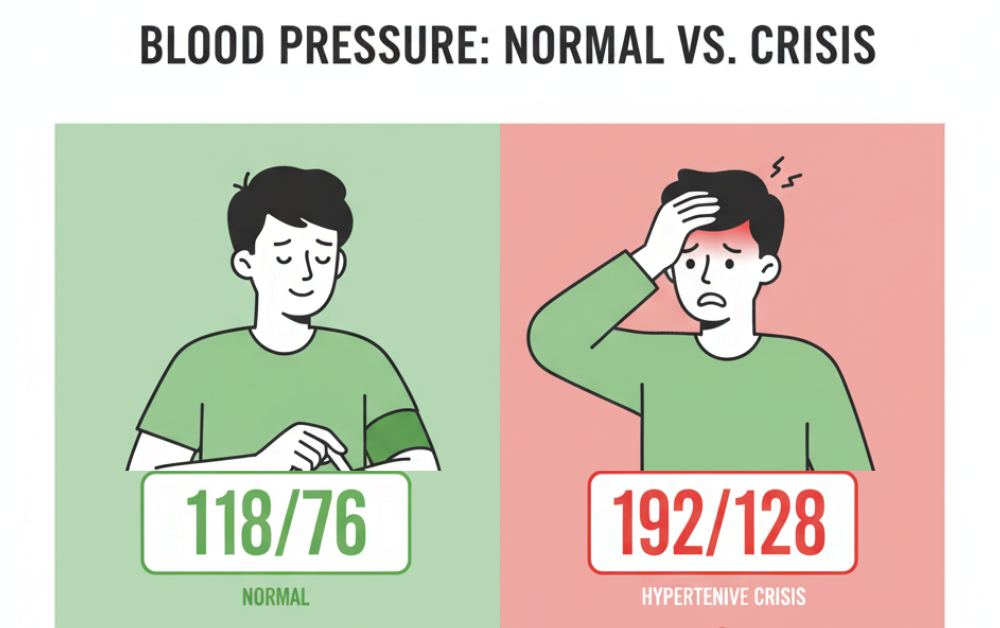
However, there are critical exceptions to this rule. When blood pressure spikes to extremely high levels—specifically above 180/120 mm Hg—headaches can occur as part of a life-threatening medical emergency called a hypertensive crisis.
In this comprehensive guide, we’ll separate fact from fiction about high blood pressure headaches, explore when headaches truly signal a blood pressure emergency, and provide evidence-based information to help you protect your health.
Understanding the Basics: Blood Pressure Explained
Before diving into the connection with headaches, let’s clarify what blood pressure means and why it matters.
What is blood pressure?
Blood pressure measures the force your blood pushes against artery walls. Systolic blood pressure (the first/top number) measures this pressure when the heart beats, while diastolic blood pressure (the second/bottom number) measures it while the heart muscle rests between beats.
Blood pressure categories:
According to the American Heart Association, blood pressure is classified as:
- Normal: Less than 120/80 mm Hg
- Elevated: Systolic 120-129 and diastolic less than 80 mm Hg
- Hypertension Stage 1: Systolic 130-139 or diastolic 80-89 mm Hg
- Hypertension Stage 2: Systolic 140 or higher or diastolic 90 or higher mm Hg
Hypertensive Crisis: Systolic higher than 180 and/or diastolic higher than 120 mm Hg
The Myth vs. Reality of High Blood Pressure Headaches
The Common Misconception
Many people believe they can “feel” when their blood pressure is high, particularly through symptoms like headaches, facial flushing, or dizziness. It’s not uncommon in hypertension practices to hear a patient say, “I can tell my pressure is high because I get a headache.”
This belief is so widespread that some people even attempt to monitor their health based on these perceived symptoms, potentially leading to dangerous delays in proper diagnosis and treatment.
What Research Actually Shows
The scientific evidence tells a different story. A study evaluating 76 patients with mild hypertension using ambulatory blood pressure monitoring found that in patients with mild hypertension, there is no association between the occurrence of headache and variation of blood pressure.
The researchers concluded that health professionals must discourage patients with hypertension from believing they can rely on the presence of headaches to know about their blood pressure levels.
The Headache Classification Committee of the International Headache Society states that mild-to-moderate hypertension does not cause headaches, though severe elevations are a different matter entirely.
When Do Blood Pressure and Headaches Connect?
While mild to moderate hypertension doesn’t typically cause headaches, the American Heart Association maintains that people do not usually experience headaches when their blood pressure is high unless it goes above a reading of 180/120 millimeters of mercury (mm Hg). At this point, it becomes a hypertensive crisis, which is a medical emergency.
Hypertensive Crisis: When Blood Pressure Becomes an Emergency
A hypertensive crisis is when blood pressure rises quickly and severely with readings of 180/120 mm Hg or higher. This dangerous condition requires immediate medical attention.
The 2024 American Heart Association scientific statement classifies severely elevated blood pressure into two categories:
- Asymptomatic Markedly Elevated Blood Pressure (formerly “Hypertensive Urgency”):
- Blood pressure readings above 180/110-120 mm Hg
- No evidence of organ damage
- Requires medical attention but not necessarily emergency room care
- Hypertensive Emergency:
- Blood pressure readings above 180/110-120 mm Hg
- WITH evidence of new or worsening target-organ damage
- Requires immediate emergency treatment
Symptoms of Hypertensive Emergency
If your blood pressure is higher than 180/120 and you are experiencing symptoms, call 911. Symptoms may include: severe headache, chest pain, shortness of breath, back pain, numbness, weakness, change in vision, or difficulty speaking.
Other warning signs include:
- Severe anxiety
- Nosebleeds
- Seizures
- Confusion or altered mental state
- Nausea and vomiting
Critical point: It is essential that people do not try to lower their blood pressure at home, even if they have the medications. Reducing blood pressure too quickly can affect the blood flow to the brain, causing unwanted side effects. Instead, they should go to an emergency room where doctors can help them lower their blood pressure in a safe, controlled environment.
The Science Behind Hypertensive Headaches
When blood pressure does reach crisis levels, how exactly does it cause headaches?
The Blood-Brain Barrier Mechanism
Many recent studies and case reports demonstrate that the pathophysiology underlying the onset of headache as it relates to abrupt rises in blood pressure seems to lie at the cellular level and mechanically becomes an issue with disruption of the blood-brain barrier.
According to research, high blood pressure can cause headaches because it affects the blood-brain barrier. In very severe cases, when blood pressure is extremely high, hypertension can result in excess pressure on the brain, which can cause blood to leak from the blood vessels in this organ. This leakage causes edema, or swelling, which is problematic because the brain sits within the skull and has no space to expand.
The swelling creates additional pressure on the brain, producing the characteristic severe headache along with other neurological symptoms.
Characteristics of Hypertensive Headaches
When headaches are truly caused by severely elevated blood pressure, they tend to have specific features:
- Location: Typically occur on both sides of the head (bilateral)
- Quality: Pulsating or throbbing pain
- Timing: Often present upon waking in the morning
- Aggravating factors: Worsens with physical activity
Associated symptoms: May be accompanied by nausea, visual changes, confusion, or other neurological signs
Common Causes of Hypertensive Crisis
Understanding what can trigger dangerous blood pressure spikes helps with prevention:
Medication-Related Causes
Missed doses: The most common cause of hypertensive crisis is forgetting to take prescribed blood pressure medications or running out of medication.
Drug interactions: The most famous agents that may cause acute pressure response include cocaine, amphetamines, oral contraceptives, and monoamine oxidase inhibitors (MAOI), especially when interacting with tyramine-containing foods.
Medication withdrawal: Hypertensive emergency may also occur following the withdrawal of beta-blockers, alpha-stimulants (e.g., clonidine), or alcohol.
Medical Conditions
Several underlying conditions can precipitate hypertensive crises:
Pheochromocytoma: Pheochromocytoma is a catecholamine-producing tumor originated from chromaffin cells that are located in the adrenal medulla and sometimes the extra-adrenal tissues. The incidence of pheochromocytoma is 0.5% in patients with hypertensive symptoms.
Preeclampsia/Eclampsia: Dangerous hypertension during pregnancy requires immediate medical intervention.
Kidney disease: Acute or chronic kidney problems can lead to severely elevated blood pressure.
Thyroid disorders: Hyperthyroidism can contribute to blood pressure spikes.
The Chronic Hypertension and Migraine Connection
While acute blood pressure spikes can cause headaches, research has also explored whether chronic hypertension increases the risk of regular headaches, particularly migraines.
What Studies Show
According to research from the Rafsanjan cohort study, hypertension was found in 24.27% of episodic primary headache cases and 31.98% of chronic primary headache cases. HTN was associated with both episodic and chronic primary headaches.
There is some controversy in the relationship between chronic hypertension and headache, particularly migraine; recent research suggests that there may be a link, but it is likely complex and multifactorial.
Possible Mechanisms
Several theories explain why people with chronic hypertension might experience more headaches:
- Shared risk factors: Obesity, sleep apnea, and metabolic syndrome increase risk for both conditions
- Vascular dysfunction: Both conditions involve blood vessel changes
- Autonomic dysfunction: Imbalances in the autonomic nervous system affect both blood pressure and headache susceptibility
- Medication effects: Some blood pressure medications can trigger headaches as a side effect
Important Distinction
Researchers followed 1,914 people with hypertension for 30 years and monitored their headaches. The results showed no link between the regular occurrence of headaches and the likelihood of cardiovascular mortality.
This means that even if you have both high blood pressure and frequent headaches, the headaches themselves don’t indicate increased heart disease risk beyond what the hypertension already confers.
Blood Pressure Treatment and Headache Relief
Interestingly, treating high blood pressure may actually reduce headache frequency for some people.
Evidence from Clinical Trials
One third fewer people reported headache in the treated group than in the placebo group when blood pressure-lowering drugs were used. There was a statistically significant reduction in the prevalence of headache in trials of each of the 4 classes of blood pressure-lowering drug.
A substudy of the Hypertension Optimal Treatment (HOT) study demonstrated that intensive blood pressure lowering significantly reduced the incidence of headache (p<0.001) while improving overall quality of life.
This suggests that while mild hypertension doesn’t cause headaches, treating elevated blood pressure might reduce headaches through other mechanisms—perhaps by improving overall vascular health or reducing other cardiovascular risk factors.
When to See a Doctor
Seek Emergency Care (Call 911) If:
Call 911 if your blood pressure is higher than 180/120 mm Hg and you have any of these symptoms: chest pain, shortness of breath, back pain, numbness, weakness, change in vision or difficulty speaking.
This is a hypertensive emergency requiring immediate hospital treatment.
Schedule Urgent Medical Attention If:
- Your blood pressure is consistently above 180/120 mm Hg but you have no other symptoms
- You’ve been diagnosed with hypertension and have sudden, severe headaches that differ from your typical headache pattern
- You experience frequent headaches along with recently diagnosed high blood pressure
- Your blood pressure medication isn’t controlling your hypertension adequately
Regular Monitoring Is Important Because:
Most people with high blood pressure have no symptoms, even if blood pressure readings reach dangerously high levels. You can have high blood pressure for years without any symptoms.
This is why the American Heart Association recommends regular blood pressure screening starting at age 18, with more frequent monitoring for those at higher risk.
Diagnosing the Cause of Your Headache
If you’re experiencing headaches and concerned about blood pressure, here’s what to expect during medical evaluation:
Initial Assessment
Blood pressure measurement: Your doctor will check your blood pressure using proper technique:
- Sitting with back supported
- Both feet flat on floor
- Arm supported at heart level
- After resting for 5 minutes
- Using appropriate cuff size
Medical history: Questions about:
- Headache characteristics (frequency, location, quality, duration)
- Medication history
- Family history of hypertension or cardiovascular disease
- Lifestyle factors (diet, exercise, stress, sleep)
- Other symptoms
Physical examination:
- Cardiovascular examination
- Neurological assessment
- Eye examination (to check for retinal changes from hypertension)
Diagnostic Tests May Include:
For suspected hypertensive emergency:
- ECG (electrocardiogram) to assess heart function
- Blood tests (kidney function, electrolytes)
- Urinalysis
- Chest X-ray
- CT or MRI scan of the brain if neurological symptoms present
For chronic hypertension evaluation:
- Ambulatory blood pressure monitoring (24-hour monitoring)
- Echocardiogram (ultrasound of the heart)
- Tests for secondary causes of hypertension
- Kidney function tests
Treatment Approaches
For Hypertensive Emergency
Hypertensive emergencies require admission to an ICU for continuous monitoring of blood pressure and target organ damage, as well as for parenteral (IV) administration of appropriate medication.
Blood pressure reduction goals:
- First hour: Reduce blood pressure by maximum 25%
- Next 2-6 hours: Lower to 160/100-110 mm Hg if patient is stable
- Following 24-48 hours: Cautiously reduce to normal levels
IV medications commonly used:
- Labetalol
- Nicardipine
- Sodium nitroprusside
- Esmolol
- Hydralazine
Critical principle: Blood pressure must be lowered gradually and carefully to avoid stroke or other complications from too-rapid reduction.
For Chronic Hypertension
Lifestyle modifications:
- Diet: DASH diet (Dietary Approaches to Stop Hypertension)
- Sodium restriction: Less than 2,300 mg daily, ideally 1,500 mg
- Regular exercise: At least 150 minutes of moderate activity weekly
- Weight management: Losing even 5-10 pounds can significantly lower blood pressure
- Limit alcohol: Maximum 2 drinks per day for men, 1 for women
- Quit smoking: Smoking raises blood pressure and increases cardiovascular risk
- Stress management: Meditation, yoga, deep breathing exercises
Medications: Common classes of blood pressure medications include:
- ACE inhibitors
- Angiotensin II receptor blockers (ARBs)
- Calcium channel blockers
- Diuretics (water pills)
- Beta-blockers
Your doctor will select medications based on your specific situation, other health conditions, and potential side effects.
For Headache Management
If headaches are related to hypertensive emergency: Treating the blood pressure crisis typically resolves the headache within hours.
If headaches are unrelated to blood pressure:
- Identify and treat the primary headache disorder (migraine, tension-type headache, cluster headache)
- Use appropriate headache medications
- Implement headache prevention strategies
- Consider whether blood pressure medications might be contributing to headaches
Prevention Strategies
Preventing hypertensive crises and managing chronic hypertension reduces all cardiovascular risks, including any potential headache connection.
Medication Adherence
Why it matters: Missing blood pressure medications is the leading cause of hypertensive crisis.
Strategies to improve adherence:
- Use pill organizers or smartphone apps with reminders
- Take medications at the same time daily, paired with another routine activity
- Keep medications visible where you’ll see them
- Set up automatic prescription refills
- Tell your doctor if side effects are bothering you—don’t just stop taking medication
- Keep a backup supply when traveling
Home Blood Pressure Monitoring
Benefits:
- Detects elevated readings between doctor visits
- Helps assess treatment effectiveness
- Provides valuable data for your healthcare team
Best practices:
- Use a validated, properly calibrated monitor
- Check at the same times daily (morning and evening)
- Take multiple readings and average them
- Keep a blood pressure log
- Important: Don’t become obsessive about checking—this can increase anxiety and blood pressure. Taking blood pressure several times a day can create anxiety that raises blood pressure.
Regular Medical Follow-Up
- Keep all scheduled appointments with your healthcare provider
- Attend follow-up visits after medication changes
- Report any concerning symptoms promptly
- Get recommended screening tests and lab work
Lifestyle Optimization
Dietary approaches:
- Follow the DASH eating plan
- Increase fruits, vegetables, and whole grains
- Choose low-fat dairy products
- Include nuts, seeds, and legumes
- Limit red meat, sweets, and sugar-sweetened beverages
Physical activity:
- Aim for at least 150 minutes of moderate aerobic activity weekly
- Include strength training twice weekly
- Find activities you enjoy to maintain consistency
- Start slowly if you’re not currently active
Stress management:
- Practice regular relaxation techniques
- Ensure adequate sleep (7-9 hours nightly)
- Maintain social connections
- Consider counseling or therapy if stress is overwhelming
Special Considerations
Secondary Headache Disorders
While we’ve focused on the relationship between blood pressure and headaches, it’s important to recognize that there are 5 major categories of secondary headaches attributed to arterial hypertension, each with validated diagnostic criteria according to the International Headache Classification:
- Headache attributed to pheochromocytoma
- Headache attributed to hypertensive crisis without hypertensive encephalopathy
- Headache attributed to hypertensive encephalopathy
- Headache attributed to pre-eclampsia or eclampsia
- Headache attributed to acute pressure response to an exogenous agent
Pregnancy and Blood Pressure Headaches
Pregnant women with severe headaches and high blood pressure require immediate evaluation, as this can signal preeclampsia or eclampsia—serious conditions threatening both mother and baby. The American Heart Association has specific guidelines for managing hypertension in pregnancy.
Morning Headaches and Sleep Apnea
It has been postulated that the morning headaches experienced by some hypertensive patients are actually due to obstructive sleep apnea. If you have morning headaches, loud snoring, and high blood pressure, ask your doctor about sleep apnea screening.
Debunking Common Myths
Myth 1: “I can feel when my blood pressure is high”
Reality: Most people cannot reliably sense their blood pressure level through symptoms. This false belief can be dangerous, causing people to delay seeking proper medical care.
Myth 2: “If I don’t have symptoms, my blood pressure must be fine”
Reality: High blood pressure is called the “silent killer” because it usually produces no symptoms until serious damage has occurred. Regular screening is essential.
Myth 3: “My blood pressure is high because I’m stressed”
Reality: While stress can temporarily raise blood pressure, chronic hypertension requires medical treatment, not just stress management alone.
Myth 4: “I can stop my blood pressure medication once my readings are normal”
Reality: Blood pressure medications control but don’t cure hypertension. Stopping medication typically causes blood pressure to rise again, potentially triggering a hypertensive crisis.
Myth 5: “Nosebleeds are a common sign of high blood pressure”
Reality: Nosebleeds are not a reliable indicator of high blood pressure except in the case of hypertensive emergency.
Living with Hypertension: Quality of Life Considerations
Having high blood pressure doesn’t mean you can’t live a full, active life. Here’s how to thrive while managing this condition:
Mental Health Support
Chronic condition management can be stressful. Consider:
- Joining support groups for people with hypertension
- Working with a therapist if health anxiety becomes overwhelming
- Practicing mindfulness and acceptance
- Focusing on what you can control
Dietary Enjoyment
Managing blood pressure doesn’t mean bland food:
- Experiment with herbs and spices instead of salt
- Discover new cuisines that naturally align with heart-healthy eating
- Find healthy versions of your favorite foods
- Allow occasional treats in moderation
Social Life
Don’t let hypertension stop you from enjoying life:
- You can still dine out—just make smart menu choices
- Moderate alcohol consumption may be acceptable (discuss with your doctor)
- Travel is possible with proper planning and medication management
- Stay active socially to support mental and physical health
The Bottom Line
The relationship between high blood pressure and headaches is more nuanced than many people realize. Here are the key takeaways:
Most important: Mild to moderate high blood pressure typically does NOT cause headaches. If you’re experiencing regular headaches, they’re likely due to other causes such as tension headaches, migraines, or stress—not your mildly elevated blood pressure.
Critical exception: When blood pressure reaches crisis levels (above 180/120 mm Hg), headaches can occur as part of a medical emergency requiring immediate treatment.
Don’t rely on symptoms: Because high blood pressure usually produces no symptoms, regular blood pressure monitoring is essential. Never assume your blood pressure is fine just because you feel okay.
Treatment benefits: Controlling high blood pressure not only reduces your risk of heart attack, stroke, and other serious complications but may also reduce headache frequency for some people.
If in doubt, get checked: If you experience a sudden, severe headache that’s different from your usual pattern, especially with other concerning symptoms, seek medical evaluation. It’s always better to be cautious.
Understanding the facts about high blood pressure headaches empowers you to take appropriate action to protect your health. Whether that means adhering to your blood pressure medication regimen, seeking emergency care for warning signs, or pursuing proper evaluation for chronic headaches, knowledge is your first line of defense.
Your heart and brain will thank you for taking high blood pressure seriously—headache or no headache.
References
- Arca KN, Halker Singh RB. The Hypertensive Headache: a Review. Current Pain and Headache Reports. 2019;23(5):30.
- Fuchs FD, Gus M, Moreira LB, et al. Behavior of ambulatory blood pressure surrounding episodes of headache in mildly hypertensive patients. Archives of Internal Medicine. 2001;161(2):252-255.
- Law MR, Morris JK, Wald NJ. Headaches and the Treatment of Blood Pressure: Results from a Meta-Analysis. Circulation. 2005;112(15):2301-2306.
- Saed D, Mohamadirizi M, Rohani M, Ansari H. Relation of hypertension with episodic primary headaches and chronic primary headaches in population of Rafsanjan cohort study. PMC. 2021.
- Rahimi-Ardabili H, Pourhoseingholi MA, Habibollahi P, Zarghi A. Secondary headaches attributed to arterial hypertension. Iranian Journal of Neurology. 2013;12(3):85-91.
- Lipsky MS, Jacobs MB. Headaches and Hypertension: Primary or Secondary? Journal of Clinical Hypertension. 2005;7(7):415-417.
- Garay-López AJ, Soto-Rivera CL. Does high blood pressure cause headaches? Myths vs. facts. Medical News Today. January 15, 2024.
- American Heart Association. When To Call 911 About High Blood Pressure. 2025.
- American Heart Association. Understanding Blood Pressure Readings. 2025.
- American Heart Association. High Blood Pressure. 2025.
- American Heart Association. Health Threats from High Blood Pressure. 2025.
- Bress AP, Anderson TS, Flack JM, et al. The Management of Elevated Blood Pressure in the Acute Care Setting: A Scientific Statement From the American Heart Association. Hypertension. 2024;81(8):e94-e106.
- Rodriguez MA, Kumar SK, De Caro M. Hypertensive Emergencies: Clinical Overview. Medscape. 2024.
- Fuchs FD, Whelton PK. Is it Time to Retire the Diagnosis “Hypertensive Emergency”? Journal of the American Heart Association. 2023;12(4):e028494.
- American Heart Association. Top 10 Things to Know About the New AHA/ACC High Blood Pressure Guideline. 2025.
- Kario K, Hess A, Bress AP, et al. 2024 AHA Scientific Statement on Management of Elevated Blood Pressure. emDocs. December 30, 2024.
- Prisant LM, Alpert BS, Robbins CB, et al. Malignant Hypertension Guidelines: Guidelines Summary. Medscape. 2024.
- Mayo Clinic Staff. High blood pressure (hypertension): Symptoms & causes. Mayo Clinic. February 29, 2024.
- Mayo Clinic Staff. Hypertensive crisis: What are the symptoms? Mayo Clinic. June 19, 2024.
- Cleveland Clinic. Can High Blood Pressure Cause Headaches? Cleveland Clinic Health Essentials. May 31, 2022.
- Excedrin. Hypertension Headache: High Blood Pressure and Headaches. 2023.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. Hypertension. 2018;71(6):e13-e115.
- National Heart, Lung, and Blood Institute. DASH Eating Plan. NIH.
- Garovic VD, Dechend R, Easterling T, et al. Hypertension in Pregnancy: Diagnosis, Blood Pressure Goals, and Pharmacotherapy. Hypertension. 2022;79(2):e21-e41.
- Arca KN, Halker Singh RB. The Hypertensive Headache: a Review. Current Pain and Headache Reports. 2019;23(5):30.
