Discovering hair loss in your child can be alarming for any parent. Whether you notice patchy bald spots, excessive shedding, or thinning hair, it’s natural to worry. The good news is that hair fall in children is more common than you might think, and most causes are treatable when properly diagnosed.
Hair loss affects an estimated 3% of pediatric office visits in the United States, and understanding the underlying cause is the first step toward effective treatment. Unlike adult hair loss, which is often related to genetics or hormones, pediatric hair loss typically has different causes and patterns.
In this comprehensive guide, we’ll explore the most common causes of hair fall in children, how to recognize different types, when to seek medical attention, and what treatments are available.
Understanding Normal vs. Abnormal Hair Loss in Children
Before diving into causes, it’s important to understand that some hair loss is completely normal.
Normal hair loss:
- Newborns naturally lose their first hair within the first few months of life, which is replaced by permanent hair
- Babies can develop bald spots from friction with crib mattresses or car seats
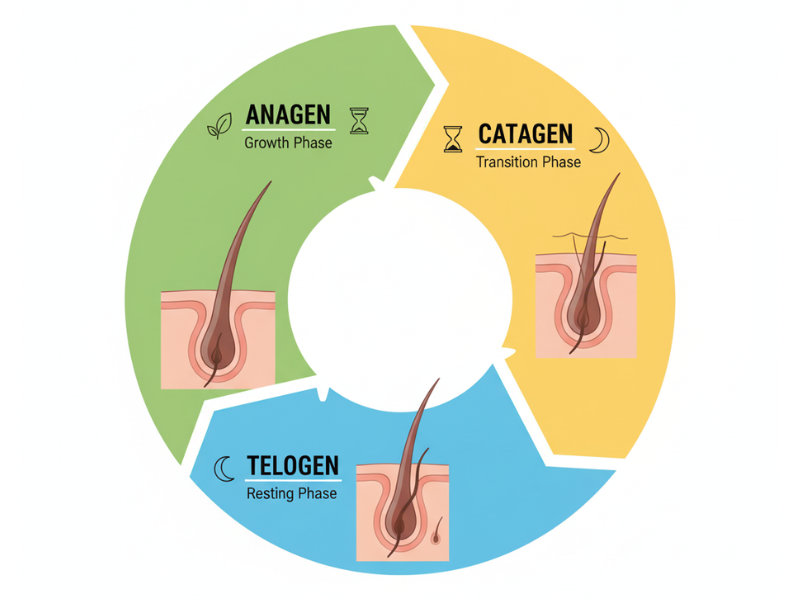
- Children naturally shed 50-100 hairs daily as part of the normal hair growth cycle
Abnormal hair loss:
- Patchy bald spots appearing suddenly
- Excessive shedding that exceeds normal daily loss
- Scaling, redness, or inflammation on the scalp
- Hair that breaks easily or has an unusual texture
- Hair loss accompanied by other symptoms (fever, fatigue, skin changes)
Common Causes of Hair Fall in Children
Hair loss in children can be classified as either acquired (develops after birth) or congenital (present from birth), and as scarring (permanent) or non-scarring (potentially reversible). Understanding these categories helps narrow down the diagnosis.
1. Tinea Capitis (Scalp Ringworm)
Tinea capitis is the most common cause of hair loss in children worldwide, particularly affecting those between 3-7 years of age.
What it is: A fungal infection of the scalp caused by dermatophyte fungi, tinea capitis is highly contagious and primarily affects children. Despite its name, it’s not caused by a worm but by microscopic fungi.
Symptoms:
- Round or oval patches of hair loss with broken hairs
- Scaly, itchy scalp with possible redness
- Black dots on the scalp where hairs have broken off
- In severe cases, painful, pus-filled swellings called kerions
- The infection can spread through direct contact, shared combs, hats, or pillows
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
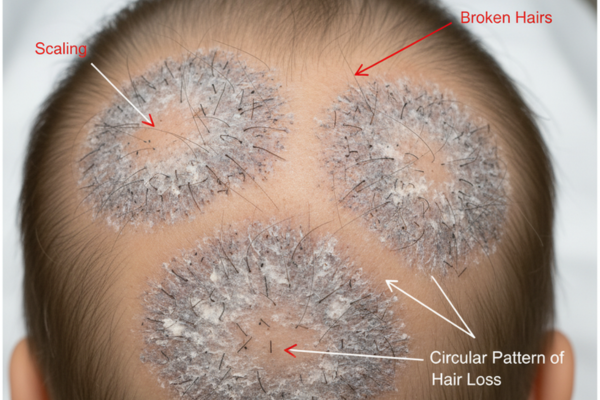
What the research says: Studies from Jordan found that tinea capitis was the most common cause of hair loss in children, accounting for 40% of pediatric hair loss cases.
Treatment: Oral antifungal medications are required, as topical treatments alone cannot penetrate the hair shaft. Common medications include griseofulvin or terbinafine, prescribed for 6-12 weeks. Medicated shampoos like ketoconazole can help reduce transmission but won’t cure the infection alone.
Prevention tip: Avoid sharing hats, brushes, combs, or hair accessories. Wash bedding and towels in hot water if a family member is infected.
2. Alopecia Areata
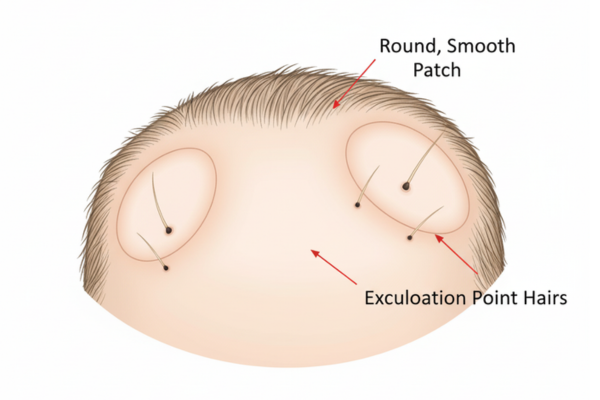
Alopecia areata is an autoimmune condition that can be particularly distressing for children and families.
What it is: The body’s immune system mistakenly attacks hair follicles, causing sudden hair loss in round or oval patches. It’s non-contagious and can affect children of any age, including infants.
Symptoms:
- Smooth, round bald patches that appear suddenly
- No scaling, redness, or broken hairs
- “Exclamation point” hairs (short hairs that are wider at the top) around bald patches
- Possible nail pitting (small dents in fingernails or toenails) in about 25% of cases
- Hair may regrow white initially before returning to normal color
What the research says: Alopecia areata was the second most common cause of pediatric hair loss in clinical studies, accounting for 26.2% of cases. The psychosocial impact of hair loss can be profound in children, making timely diagnosis and support essential.
Treatment options: There is no cure for alopecia areata, but several treatments can help:
- Topical corticosteroids: First-line treatment for young children due to ease of use and safety
- Intralesional corticosteroid injections: Effective for localized patches in older children who can tolerate injections
- Topical immunotherapy: For extensive cases, though requires specialized monitoring
- JAK inhibitors: Newer oral medications showing promise but still being studied in pediatric populations
Important note: Many children experience spontaneous regrowth within a year, though recurrence is common. Psychological support is crucial as hair loss can significantly impact self-esteem and social interactions.
3. Telogen Effluvium
Telogen effluvium is a stress-related form of hair loss that causes widespread shedding.
What it is: This condition occurs when a stressful event interrupts the normal hair growth cycle, causing large numbers of hair follicles to enter the resting (telogen) phase simultaneously. Hair falls out 2-3 months after the triggering event.
Common triggers in children:
- High fever or severe illness
- Surgery or hospitalization
- Significant emotional stress (family death, trauma, major life changes)
- Nutritional deficiencies (iron, zinc, protein)
- Certain medications
- Rapid weight loss
Symptoms:
- Diffuse hair thinning across the entire scalp
- Increased hair shedding when brushing or washing
- No bald patches or broken hairs
- Noticeable thinning at the temples and frontal hairline
What the research says: Telogen effluvium accounted for 17.6% of pediatric hair loss cases in epidemiological studies, with common causes being frequent illnesses with high-grade fever and iron deficiency anemia.
Treatment: The good news is that telogen effluvium is usually temporary and self-resolving:
- Identify and treat the underlying cause
- Correct any nutritional deficiencies
- Manage stress and anxiety
- Be patient – hair regrowth typically occurs within 6-12 months at a rate of about 1 cm per month
- No specific medications are usually required
4. Traction Alopecia
Traction alopecia results from prolonged or repeated pulling on the hair.
What it is: Hair loss caused by tension and pulling on hair follicles from tight hairstyles like ponytails, braids, buns, or hair extensions.
Symptoms:
- Hair loss concentrated where tension is greatest (hairline, temples, crown)
- Small bumps or pimples on the scalp
- Redness and tenderness in affected areas
- Broken hairs of varying lengths
- Initially non-scarring, but can become permanent if the practice continues
High-risk hairstyles:
- Very tight ponytails or buns
- Tight braids or cornrows
- Hair extensions, especially if poorly applied
- Excessive use of hair accessories with tight grips
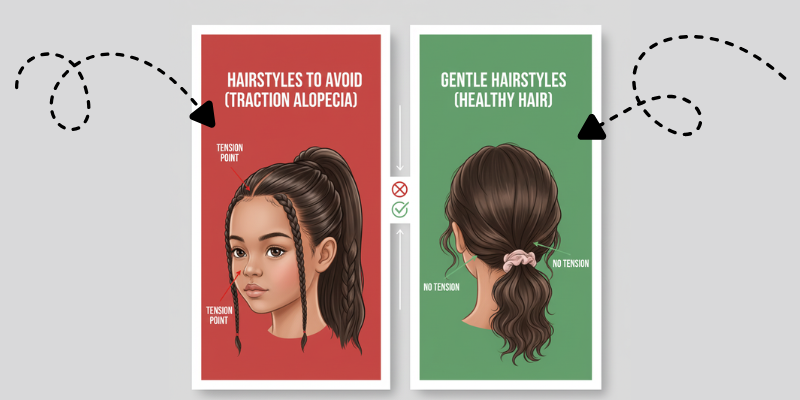
What the research says: Traction alopecia is one of the most prevalent causes of hair loss in children and is entirely preventable with proper hair care practices.
Treatment and prevention:
- Switch to looser hairstyles immediately
- Avoid chemical treatments and heat styling
- Let hair down whenever possible
- Use soft hair ties without metal
- Seek alternatives like protective styles that don’t pull on roots
- If caught early, hair typically regrows within months once tension is removed
5. Trichotillomania (Hair-Pulling Disorder)
Trichotillomania is a psychological condition where children compulsively pull out their own hair.
What it is: A disorder characterized by recurrent hair pulling resulting in noticeable hair loss, often triggered by stress, anxiety, or boredom.
Symptoms:
- Patchy, irregular hair loss with broken hairs of different lengths
- Hair loss often on the scalp, but can also affect eyebrows and eyelashes
- The pattern doesn’t match typical medical causes
- Child may deny hair pulling initially
- More common in older children and adolescents
Associated factors:
- Anxiety, depression, or obsessive-compulsive tendencies
- Stress at home or school
- Perfectionism or need for control
- Family history of similar behaviors
Treatment approach: This condition requires a multi-faceted approach:
- Cognitive-behavioral therapy (CBT): The most effective treatment, helping children recognize triggers and develop alternative behaviors
- Habit reversal training: Teaching awareness and competing responses
- Stress management techniques: Relaxation exercises, mindfulness
- Family therapy: Addressing environmental stressors
- Medication: In some cases, SSRIs may be prescribed for underlying anxiety
Important consideration: Approach the situation with compassion and without blame. Hair pulling is often involuntary or semi-voluntary, and punishment is ineffective.
6. Nutritional Deficiencies

Inadequate nutrition can significantly impact hair health in growing children.
Key nutrients for healthy hair:
Iron: Iron deficiency is one of the most common nutritional causes of hair loss in children, particularly in developing countries. Iron is essential for oxygen transport to hair follicles.
Zinc: Studies have identified zinc deficiency as a cause of chronic diffuse hair loss in children, even in the absence of other characteristic signs of zinc deficiency. Zinc supports hair tissue growth and repair.
Protein: Hair is primarily made of keratin, a protein. Severe protein malnutrition can lead to hair thinning, texture changes, and hair loss.
Vitamin D: Vitamin D plays a role in creating new hair follicles and regulating the hair growth cycle.
Biotin (Vitamin B7): While biotin deficiency is rare, it can cause hair loss when present, particularly in children with absorption disorders.
Symptoms of nutritional deficiency-related hair loss:
- Diffuse hair thinning across the scalp
- Dry, brittle hair texture
- Slow hair growth
- Changes in hair color or texture
- May be accompanied by other symptoms: fatigue, pale skin, poor wound healing
What the research says: A comprehensive review found that micronutrients such as vitamins and minerals play an important role in normal hair follicle development, and deficiency of such micronutrients may represent a modifiable risk factor in hair loss.
Treatment:
- Blood tests to identify specific deficiencies
- Dietary counseling and meal planning
- Targeted supplementation under medical supervision
- Monitor levels to avoid over-supplementation, which can be harmful
- Address underlying absorption issues if present
Foods rich in hair-healthy nutrients:
- Iron: Red meat, spinach, lentils, fortified cereals
- Zinc: Meat, shellfish, legumes, seeds, nuts
- Protein: Lean meats, fish, eggs, dairy, beans
- Vitamin D: Fatty fish, egg yolks, fortified milk
Biotin: Eggs, nuts, sweet potatoes, avocados
7. Thyroid Disorders
Though less common, thyroid problems can cause hair loss in children.
What it is: Hypothyroidism, a condition where the thyroid gland is underactive and produces insufficient thyroid hormones, can lead to hair loss in children.
Symptoms:
- Diffuse hair thinning
- Dry, coarse hair texture
- Accompanied by: fatigue, weight gain, cold intolerance, constipation, slowed growth
- Brittle nails
- Dry skin
Diagnosis: Blood tests measuring TSH (thyroid-stimulating hormone), T3, and T4 levels.
Treatment: Thyroid hormone replacement therapy (levothyroxine) prescribed and monitored by a pediatric endocrinologist. Hair typically regrows once thyroid levels are normalized.
8. Other Medical Causes
Several other conditions can cause hair loss in children:
Bacterial infections:
- Folliculitis or other scalp infections can cause temporary hair loss
- Treated with antibiotics
Lupus (Discoid Lupus Erythematosus):
- Can cause scarring alopecia in children
- Requires rheumatological evaluation and treatment
Chemotherapy or radiation:
- Cancer treatments commonly cause temporary hair loss
- Hair typically regrows after treatment ends, though texture may change
Hair shaft abnormalities:
- Genetic conditions affecting hair structure (e.g., monilethrix, pili torti)
- Often present from birth or early childhood
- May require specialized genetic testing
When to See a Doctor
While some hair loss resolves on its own, certain situations require prompt medical evaluation:
Seek medical attention if your child experiences:
- Sudden or rapid hair loss
- Large bald patches or extensive thinning
- Hair loss with scalp scaling, redness, swelling, or pus
- Hair loss accompanied by other symptoms (fever, rash, fatigue, weight changes)
- Hair loss causing significant emotional distress
- Eyebrow or eyelash loss
- Hair that breaks easily or has an unusual texture
- No improvement after 3-6 months
Diagnostic Approach
When you visit a healthcare provider for your child’s hair loss, expect a thorough evaluation:
Medical history:
- When hair loss began and how it has progressed
- Family history of hair loss or autoimmune conditions
- Recent illnesses, medications, or stressful events
- Dietary habits and potential nutritional deficiencies
- Hair care practices and styling habits
Physical examination:
- Scalp examination for patterns of hair loss, scaling, inflammation, or scarring
- Hair pull test to assess active shedding
- Examination of other body areas for additional hair loss
- Check for nail changes
- General physical examination
Diagnostic tests may include:
- KOH preparation: Microscopic examination for fungal infections
- Fungal culture: To identify specific dermatophyte species
- Dermoscopy: Magnified examination of the scalp and hair
- Blood tests: Complete blood count, ferritin, zinc, vitamin D, thyroid function
- Scalp biopsy: Rarely needed, but can help diagnose scarring alopecias or unusual cases
- Hair mineral analysis: Not routinely recommended due to questionable accuracy
Treatment Overview by Cause
Evidence-based treatment approaches for common causes of hair fall in children
| Condition | Primary Treatment | Expected Outcome |
|---|---|---|
| Tinea Capitis | Oral antifungal medication (6-12 weeks) | Full regrowth expected |
| Alopecia Areata | Topical/intralesional corticosteroids | Variable; many regrow within a year |
| Telogen Effluvium | Treat underlying cause; nutritional support | Resolves within 6-12 months |
| Traction Alopecia | Change hairstyles; reduce tension | Regrowth if caught early |
| Trichotillomania | CBT, behavioral therapy | Good with appropriate mental health treatment |
| Nutritional Deficiency | Dietary changes; targeted supplementation | Gradual improvement over months |
| Hypothyroidism | Thyroid hormone replacement | Regrowth once levels normalized |
Outcome Indicators:
Treatment timelines are approximate and may vary based on individual response, severity of condition, and adherence to treatment plans. Always consult with a qualified pediatric dermatologist or healthcare provider for accurate diagnosis and personalized treatment recommendations.
Emotional and Psychological Support
The psychological impact of hair loss on children should never be underestimated.
Common emotional challenges:
- Low self-esteem and poor body image
- Social withdrawal or school avoidance
- Bullying or teasing from peers
- Anxiety and depression
- Impact on family relationships
Supporting your child:
- Acknowledge their feelings without minimizing concerns
- Educate them about their condition in age-appropriate terms
- Connect with support groups for children with hair loss
- Consider counseling or therapy if emotional distress is significant
- Explore temporary solutions: hats, headbands, wigs, or hairpieces if desired
- Work with school to prevent bullying and create a supportive environment
Resources:
- Children’s Alopecia Project: Provides support and resources for families
- National Alopecia Areata Foundation: Educational materials and community connection
- School counselors and psychologists
Prevention Strategies
While not all causes of hair fall in children are preventable, some measures can help:
General hair health:
- Use gentle, age-appropriate hair care products
- Avoid excessive heat styling, chemical treatments, and harsh brushing
- Choose soft hair ties and avoid overly tight hairstyles
- Protect hair from excessive sun exposure
- Ensure adequate nutrition with a balanced diet
Preventing infection:
- Don’t share hats, brushes, combs, or hair accessories
- Teach children proper hygiene
- Treat pets with ringworm promptly
- Wash bedding and towels regularly
Stress management:
- Maintain open communication about feelings and worries
- Encourage healthy coping mechanisms
- Ensure adequate sleep and physical activity
- Create a stable, supportive home environment
Prognosis: What to Expect
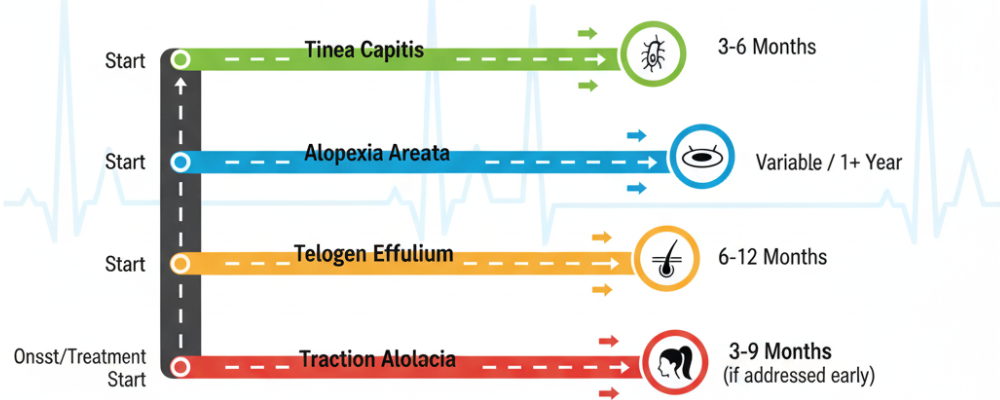
The outlook for hair fall in children is generally positive:
Non-scarring alopecia: The majority of pediatric hair loss cases are non-scarring, meaning hair follicles remain intact and hair has the potential to regrow.
Timeline for regrowth:
- Tinea capitis: 3-6 months after successful treatment
- Alopecia areata: Highly variable; many see regrowth within a year
- Telogen effluvium: 6-12 months after trigger is removed
- Traction alopecia: Months to a year if tension is eliminated early
- Nutritional deficiencies: Gradual improvement over 3-6 months with correction
Factors affecting prognosis:
- Early diagnosis and treatment
- Adherence to treatment plans
- Severity and extent of hair loss
- Underlying cause
- Individual response to treatment
The Bottom Line
Hair fall in children can be concerning, but it’s important to remember that most causes are treatable and reversible. Accurate diagnosis of hair loss in children is of major significance as it can have severe psychological implications given the cosmetic importance of hair.
If you notice unusual hair loss in your child, don’t wait to seek evaluation. Early diagnosis and treatment can prevent progression, minimize scarring in certain conditions, and reduce the emotional impact on your child.
With proper medical care, nutritional support, and emotional encouragement, most children with hair loss can look forward to healthy hair regrowth and restored confidence.
Remember: You’re not alone in this journey. Healthcare providers, support groups, and resources are available to help your child through hair loss challenges and toward a positive outcome.
References
- Xu L, Liu KX, Senna MM. A Practical Approach to the Diagnosis and Management of Hair Loss in Children and Adolescents. Frontiers in Medicine. 2017;4:112.
- Al-Refu K. Hair Loss in Children: Common and Uncommon Causes; Clinical and Epidemiological Study in Jordan. International Journal of Trichology. 2013;5(4):185-189.
- Shetty VM, Shenoi SD, Chavan P, Kushwaha RS. Hair Loss in Children: A Clinicoetiological Study from South India. International Journal of Trichology. 2021;13(6):231-235.
- Koblinski JE, O’Haver JA, Andrews ID. An Approach to Hair Loss in Pediatric Primary Care. Journal of Pediatric Health Care. 2021;35(5):535-548.
- Imhof RL, Davis DMR, Tollefson MM. Hair Loss. Pediatrics in Review. 2020;41(11):570-584.
- American Academy of Pediatrics. Hair Loss (Alopecia) in Children. 2024.
- WebMD Medical Reference. Hair Loss in Children: Causes and Treatment. Updated September 2, 2024.
- Al-Refu K, Goodfield M. Hair Loss in Children: Etiologies and Treatment. IntechOpen. 2017.
- Children’s Hospital. Pediatric Alopecia: Causes, Diagnosis, and Treatment. Children’s Health. 2025.
- Castelo-Soccio L. Diagnosis and Management of Alopecia in Children. Pediatric Clinics of North America. 2014;61(2):427-442.
- Tosti A, Bellaney GJ, Iorizzo M. Alopecia Areata: A Long-Term Follow-up Study of 191 Patients. Journal of the American Academy of Dermatology. 2006;55(3):438-441.
- Chan YC, Tay YK. Approach to a Child with Hair Loss. Singapore Medical Journal. 2019;60(3):116-120.
- Guo EL, Katta R. Diet and Hair Loss: Effects of Nutrient Deficiency and Supplement Use. Dermatology Practical & Conceptual. 2017;7(1):1-10.
- Almohanna HM, Ahmed AA, Tsatalis JP, Tosti A. The Role of Vitamins and Minerals in Hair Loss: A Review. Dermatology and Therapy. 2019;9(1):51-70.
- Harvard Health Publishing. Vitamins, Minerals, and Hair Loss: Is There a Connection? Harvard Medical School. Updated April 22, 2024.
- Trost LB, Bergfeld WF, Calogeras E. The Diagnosis and Treatment of Iron Deficiency and Its Potential Relationship to Hair Loss. Journal of the American Academy of Dermatology. 2006;54(5):824-844.
- Rasheed H, Mahgoub D, Hegazy R, et al. Serum Ferritin and Vitamin D in Female Hair Loss: Do They Play a Role? Skin Pharmacology and Physiology. 2013;26(2):101-107.
- Park SY, Na SY, Kim JH, et al. Iron Plays a Certain Role in Patterned Hair Loss. Journal of Korean Medical Science. 2013;28(6):934-938.
- Karashima T, Tsuruta D, Hamada T, et al. Oral Zinc Therapy for Zinc Deficiency-Related Telogen Effluvium. Dermatologic Therapy. 2012;25(2):210-213.
- Sanad EM, Elrashied R. Evaluation of Serum Ferritin and Vitamin D Levels in Females with Diffuse Hair Loss. Journal of Cosmetic Dermatology. 2020;19(11):2918-2922.
- Chen X, Yang M, Cheng L. Systemic Antifungal Therapy for Tinea Capitis in Children. Cochrane Database of Systematic Reviews. 2016;2016(5):CD004685.
- Gupta AK, Drummond-Main CE, Cooper EA, et al. Systematic Review of Nondermatophyte Mold Onychomycosis: Diagnosis, Clinical Types, Epidemiology, and Treatment. Journal of the American Academy of Dermatology. 2012;66(3):494-502.
- Pratt CH, King LE Jr, Messenger AG, et al. Alopecia Areata. Nature Reviews Disease Primers. 2017;3:17011.
- Gilhar A, Etzioni A, Paus R. Alopecia Areata. New England Journal of Medicine. 2012;366(16):1515-1525.
- Strazzulla LC, Wang EHC, Avila L, et al. Alopecia Areata: Disease Characteristics, Clinical Evaluation, and New Perspectives on Pathogenesis. Journal of the American Academy of Dermatology. 2018;78(1):1-12.
